Share

OSTEOPOROSIS
By Victoria Healthcare 12 April 2019
Osteoporosis is a disease that results in the loss of bone tissue. When bone tissue is lost, the bones become brittle and break more easily.
Signs
The bone loss of osteoporosis often causes no signs. People may not know that they have the disease until their bones become so weak that a sudden strain, bump or fall causes a bone to break.
Bone loss that causes bones in the spine to collapse may be felt or seen as severe back pain, loss of height, stooped posture or a hump.

Risk Factors
Women, in general, have less total bone mass than men, making them more likely to have osteoporosis. When you have one or more of these risk factors, you may be at greater risk for osteoporosis.
You have:
+Reached menopause before age 45
+Elderly women in your family who had fractures
+Had broken bones
+Conditions such as an endocrine disease, rheumatoid arthritis, kidney disease or Cushing’s disease
+Had cancer treatments
Other risk factors include:
+Eating disorder such as anorexia – current or in the past
+Low calcium intake or vitamin D deficiency
+Low body weight or small bone body structure
+Caucasian or Asian
+Advanced age
+Unhealthy lifestyle behaviors, such as smoking, drinking a lot of alcohol and/or caffeine, and not getting enough exercise
+Certain medicines such as corticosteroids or heparin (long-term) Tests
Talk to your doctor about testing for osteoporosis. Your doctor may order these and other tests:
- Bone mineral density test – This x-ray test measures bone density in the lower spine, hip or wrist. The most common type of this test is a dual-energy x-ray absorptiometry (DXA) scan. The test is painless and only takes a few minutes. The results of the scan are reported as the amount of bone loss.
- Blood and urine tests to check hormone levels and look for other conditions that increase bone loss such as vitamin or mineral deficiency.
Your Care
Start at an early age to prevent and treat osteoporosis. Keep your bones strong throughout your life. Treatments can help stop or slow down further bone loss and bone breaks, but there is no cure.
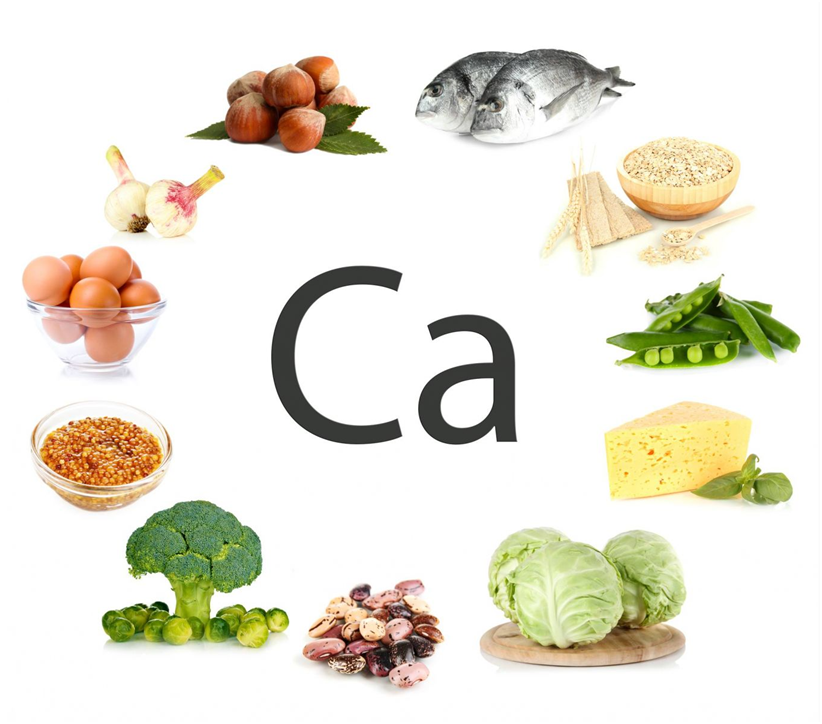
- Eat a diet high in calcium or take calcium supplements each day.
+For adults 19 to 50 years of age, eat 3 servings or 1000 milligrams (mg) of calcium each day.
+For men over 50 years of age, eat 3 servings or 1000 mg of calcium each day.
+For men over 70 years of age, eat 4 servings or 1200 mg of calcium each day.
+For women over 50 years of age, eat 4 servings or 1200 mg of calcium each day.
+Sources of calcium in foods include milk, dairy products or calcium-fortified foods such as juices or cereals.
+Calcium supplements may be an option if you cannot get enough calcium in your diet.
+Do not increase your calcium intake above the advised amount.
+Vitamin D helps your body absorb calcium. The main source of vitamin D for most people is sunshine. For people with lightcolored skin, 15 to 20 minutes of sun exposure a day is enough for the body to make vitamin D. For people with dark-colored skin, 30 minutes a day is needed. If you cannot get enough sunlight, take 600 International Units (IU) per day for ages 1 to 70 years and 800 IU per day for ages 71 years and older.
- Maintain a healthy weight. Being underweight puts you at higher risk for osteoporosis.
- Perform standing exercises such as walking, jogging, dancing and aerobics 3 to 4 hours per week.
- Stop smoking or using tobacco.
- Limit alcohol, caffeine and carbonated drinks.
- Talk to your doctor about medicines to reduce bone loss.
- Ask your doctor about estrogen replacement therapy if you are going through menopause or have had your ovaries removed. Estrogen can prevent more bone loss, but there are risks with this treatment. Talk to your doctor about the risks and benefits.
Talk with your doctor or nurse if you have any questions or concerns.


